
Chat-GTP-generated Mojo Dojo Casa House of Healthcare for Women
Key Takeaways:
- Healthcare is supposed to be … Barbie Land as women steer the majority of healthcare decisions, purchases, and interactions today. Yet, our healthcare system is a Mojo Dojo Casa House that, while leaning heavily on women’s contributions, has consistently overlooked women’s health issues, amplifying the burden on women as caregivers.
- To close the gender care gap requires funding, innovation and focus across infrastructure and access solutions across women’s interaction with healthcare as patients and as caregivers beyond just fertility.
- By recognizing the power of female decision-makers in healthcare and their unique challenges, healthtech founders can tap into the female engine of product-led growth.
- “A women’s health is her capital”. Investing in women and women’s founders start with investing in healthcare.
Introduction
2023 is the year of womanhood & girlhood. This year was epitomized by the blockbuster sensation “Barbie,” alongside the cultural titans of Taylor Swift’s Eras Tour and Beyoncé’s Renaissance Tour. It was a year that celebrated the formidable power of women, showcasing their immense influence and the pivotal role of female capital in propelling the entire economy forward, even leaving its mark on the NFL.
This was the year when women were heralded as powerhouses—transformative artists, discerning consumers, visionary leaders, and astute businesswomen. This was the year as if the world finally woke up to the strength and influence of women, highlighting their indelible contributions and the burden they shoulder. In healthcare, women’s unmistakable impact not only shaped the market but also steered the majority of healthcare decisions, purchases, and interactions.
Before we dive in, true to our OCV’s style as we are headquartered in Los Angeles, the entertainment capital of the world, and true to the author’s (clinical) admiration for Taylor Swift, each section alternative’s title is appropriately a title of Ms. Swift’s song.
Are you …. Ready for It?
Quick Facts – Look what you made me do!
As Care Givers and as Patients:
- Women are responsible for 80% of family healthcare decisions
- Women purchased 93% all over-the-counter pharmacy items compared to men
- Women spend 38% more on healthcare per capital during their lifetime (and nearly 80% during their reproductive year)
- Women are 75% more likely than men to use digital health apps and tools
- Upwards of 75% of all caregivers are females who spent 50% more than their male counterparts to provide unpaid care to loved ones
A common thread we observe is that women stand at the forefront as the principal decision-makers, the primary audience, and the central figures in the majority of healthcare communications—even when these messages aren’t explicitly directed at them. If our economy and healthcare system were to be personified, they would undoubtedly embody the female essence. Healthcare should be…. Barbie land.
Yet, paradoxically, just like the Kens overtook Barbie land, mistreated the Barbies, and turned it into a Mojo Dojo Casa House of horses, our healthcare system that leans heavily on women’s contributions has consistently overlooked women’s health issues, amplifying the burden on women as caregivers.
The initial step towards mending the fractures within the U.S. healthcare industry begins with reevaluating and transforming our system’s engagement with women.
Because it’s no secret to anybody, there is a lot of Bad Blood.
I. The ABC Gender Gap in HealthCare – Death by a Thousand Cuts
1. The Access Gap – Blank Space
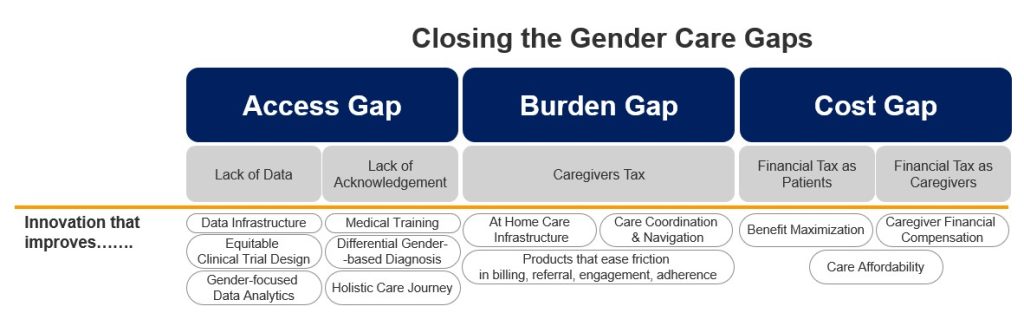
The last few decades have witnessed groundbreaking advancements in biomedical and technological innovation that significantly extended life expectancy across the globe. However, this remarkable transformation has conspicuously overlooked the unique health conditions and diseases affecting women, spanning the entire spectrum of the biomedical innovation and healthcare value chain. At the heart of this oversight lie deep-seated gender access gaps, rooted in two primary issues:
- The Lack of Women’s Health Data: leads to the lack of attention to innovation for women’s indications
- The Lack of Acknowledgment: leads to poor clinical quality for female patients in the healthcare systems.
A. The lack of data: No body (data), no crimes
Shortcomings across gender data definition, generation, aggregation, and analysis heavily impacted women’s health. Mckinsey’s reports on women’s health (2023 and 2024) provided a comprehensive look at the issues.
- Definition: Women’s health has been largely defined as “reproductive health” for most of modern medicine up until the last decades in 2000. Don’t say I didn’t, say I didn’t warn ya that women’s health doesn’t just evolve by her reproductive function!
- Data Generation, Aggregation & Analysis: The gaps across the data value-chain truly undermine the visibility and ability to accurately reflect the prevalence and burden of women’s health conditions. I got a blank space… And I (won’t) write your name!
With the blank spaces across women’s health data, the entire industry has approached women’s health as the Titanic captain scoffing at the tip of the iceberg. As most innovations in biomedical research are funded by governmental and private investments, the lack of data and data infrastructure substantiates a complete ignorance to support innovation toward women’s conditions. This resulted in just 5% of biopharma pipeline assets and only 4% of medtech approvals addressing women’s health conditions with 80% of those assets focused on oncology indications. To make matters worse, outside of female-specific health conditions, the lack of data on sex differences between indications across drug development & commercialization is astonishing with only 1/4 of clinical trials in the US having sex-disaggregated data with most failing to consider differences between sexes. This resulted in women being widely overmedicated and suffering from excess side effects because drug doses were calculated based on studies done overwhelmingly on male patients.
Truly and literally, death by a thousand cuts!
B. The Lack of Acknowledgement – I Forgot You Existed!
All the gaps of data in women’s health directly how women are treated as patients. From lack of diagnosis to delayed treatment to dismissed suffering, our healthcare system stays true to the sentiment of “I forgot that you existed. It isn’t love, it isn’t hate. It’s just indifference”
- Diagnosis Gap: Lack of data, understanding & acknowledgment of differential symptoms manifestation in women vs men led to a 7x higher risk for women to be misdiagnosed and discharged while having a heart attack. A large cohort study showed women were diagnosed later than men in 700 diseases. That includes 2.5 more years for cancer, and 4.5 years for diabetes, and more than 50% of women living with endometriosis remain undiagnosed. This given the fact that women are more likely than men to seek out care makes this gender gap of underdiagnosis more alarming. Almost every woman has a personal anecdote about how their health concerns were ignored or deflected towards “hysterical” or “psychological” causes by their providers. The gender gap and barrier to care is even worse for women of color as highlighted in our previous OCV Insights Post.
- Treatment Gap: As someone who fainted on my way out of the clinic after being briskly dismissed with two Tylenol after an IUD procedure, I came to the stark realization of our system’s abhorrent handling of female pain: our pain sensitivity, our propensity to report pain, and our tolerance levels. And I knew I wasn’t the only one. A glaring statistic is found in research showing that merely 50% of women who undergo coronary bypass surgery are prescribed painkillers and women endure a distressing wait of 65 minutes on average before receiving analgesics for acute pain in emergency rooms (vs 49 minutes for men). The neglect in pain management is profoundly exacerbated for African American women, where deeply ingrained racial bias. Pain is just a glaring example of many, many inequalities of care women face, from the abysmal maternal care outcome to other OB/GYN conditions, to diabetes, GIs.
2. The Burden Gap – (Can’t) Shake it Off
Another interaction women have with our healthcare system that often is not discussed is their role as caregivers. An estimated 66% of caregivers are female with women spending as much as 50% more time providing care than male caregivers. Approximately 80% of women are the primary healthcare decision-makers for their families. Mothers are more likely than fathers to take their children to doctor visits, making up 65% of all pediatric appointments. This isn’t a surprise as women cannot shake it off the heavier burden of “Chief Medical Officer” when it comes to caregiving responsibilities. All that came at a cost as women have to spend a substantial amount of time & effort to navigate the complexity of a broken US healthcare system: from appointment transportation, insurance reimbursement, bill payments, hospitalization care, and specialist referrals on top of their other responsibilities like career, childcare, jobs, and their health.
The Health Tax of Caregivers: The role of a caregiver, not only sets women back by its financial burdens but also places physical and mental tolls on one’s health. Caregivers are six times more likely to grapple with depression, anxiety, and other stress-induced health issues. More than 50% of caregivers have been diagnosed with two or more chronic conditions (14% higher than the general US adult population) and 25% of women caregivers report health complications directly linked to the caregiving duties. 21% of female caregivers receive mammograms less frequently, while a staggering two-thirds of older women neglect preventive health services, due to both lack of access and cost. This data not only sheds light on the urgent need for comprehensive support systems for caregivers but also calls for a broader recognition of the sacrifices they make, often at the expense of their health.
3. The Cost Gap – All (not) Too Well
As patient:
Being a woman is costly! It is no secret that women’s healthcare costs are substantially higher than that of our male counterparts as the so-called “Pink Tax” is far more reaching than most people realize. Women face a disproportionate financial burden in healthcare compared to men, a disparity that extends across various stages of life and medical needs. Adult women incur nearly twice the annual health expenditures of their male counterparts. This financial strain continues into later life, as older women on Medicare exhibit significantly lower savings while grappling with higher out-of-pocket expenses. Nearly 30 percent of women cannot afford their prescribed medications annually. High drug prices exacerbate this issue, as seen with Herceptin, a breast cancer medication whose price surged by 78 percent from 2005 to 2017. Breast cancer stands as one of the costliest conditions, with medication expenses topping treatment costs. Moreover, significant price hikes in drugs like Millicent’s Femring and Teva’s Prefest emphasize the broader impact of rising drug costs on women, including those requiring medications not traditionally associated with women’s health, such as diabetes treatments. This begs for the need for a critical examination of healthcare and medication pricing policies to address the disproportionate financial burden on women.
As caregivers:
Financially, the impact is significant for women caregivers as they often face economic hardships due to their caregiving responsibilities. 33% of working women decreased their work hours and assignments to perform unpaid care for loved ones. AARP research indicates that female caregivers can lose up to $324,044 in wages and benefits over a lifetime due to caregiving duties. Outside of the hours lost from workforce participation mostly to navigate the healthcare systems, women suffer tremendous impact from the cost of caregiving itself. Whether it’s dealing with expensive prescriptions, installing wheelchair ramps for their loved ones, or managing other medical equipment. Unpaid caregiving women are more likely to live in poverty compared to non-caregivers.
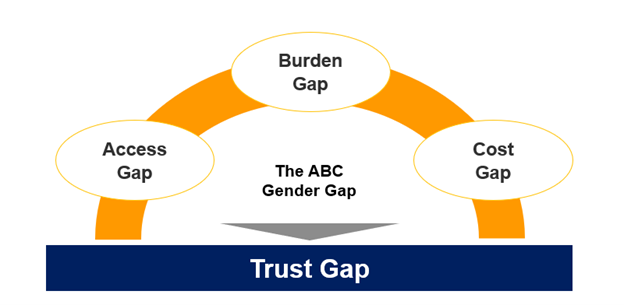
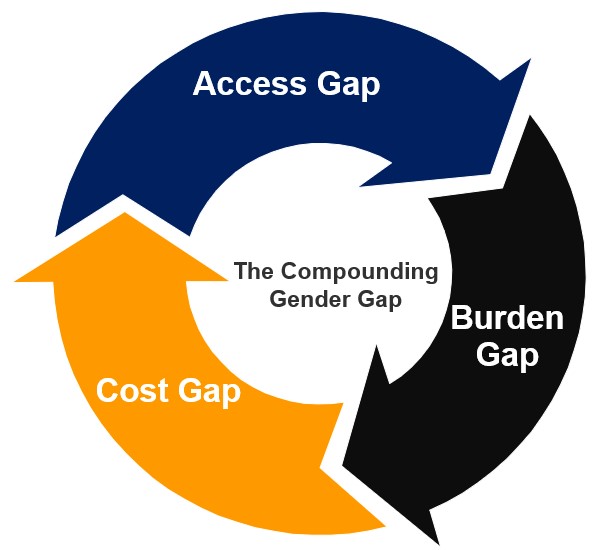
In Summary, the Access, Burden, and Cost (ABC) Gaps above created a profound Trust Gap women harbor towards a healthcare system that is supposed to safeguard them. This presented a vicious cycle that every interaction women face as caregivers and as patients with the Mojo Dojo Casa House which is the US healthcare system leaving them worse off financially, emotionally, mentally, and physically.
II. Closing the Gaps – Are we out of the woods?
Women’s health has come into focus in the last few years, especially since the overturn of Rode v.Wade. Increased legislation, bills, and federal and private funding programs for women’s health research and care delivery have been a much-needed and encouraging sign.
The fast-growing FemTech space with increased private equity and venture capital funding here is a testimony of a potential changing tide with $481M VC funding towards women’s health in 2023. Yet the majority of those funding still focused on fertility, pregnancy, and oncology.
To close the gaps in women’s health, funding needs to be funneled towards both infrastructure & engagement across the ABC Gaps. Infrastructures to improve the lack of comprehensive & accurate human data, equitable trial design, and additional financial infrastructure to remove financial and health burdens on caregivers are essential. Improving women’s experience and engagement with the system requires not only innovation in diagnosis and treatment through gender-focused medical training but also a more holistic care journey and access to care across conditions.
The Female Engine of Product-Led-Growth
Outside of identifying the best innovative solution, I would love to encourage founders to lean into the formidable force of the female engine of product-led growth.
At OCV, we have been championing product-led growth companies— ones that eschew the need for expansive sales forces and hefty marketing budgets, favoring organic growth through word-of-mouth instead.
Guess who holds the multiplier effect in the economy and healthcare? Women! Recognizing that women are the primary recipients, audience, and drivers of every healthcare interaction and value chain, how would healthtech innovators leverage this insight to recalibrate their product and growth strategies? By deeply understanding the audience—their inequalities, burdens, and challenges as patients and caregivers—and tailoring product and business models to align with their needs and values, startups can craft intuitive solutions that leverage the intrinsic power of women in healthcare, setting themselves apart and fueling accelerated growth.
And no, pink is not the strategy! Though, admittedly, that might appeal to some, myself included. It’s about delving into a profound understanding of women and their needs as meticulously as you would any new market. A great example here is KindBody who had built authentic brand and product through constructive communication that tailored uniquely to their key demographics.
However, this concept of the female engine behind product-led growth is not limited to companies working directly on women’s conditions. This should apply to almost every company in healthcare whose audience is disproportionate women as patients and as caregivers: that extends to prior authorization, medication adherence, payments, clinical navigation, pharmacy engagement, and care affordability. This encourages out-of-the-box strategies to engage women across the care journey. This might involve assembling a diverse team with executive women at the helm who grasp the core needs of your female audience. It means meeting women where they are and acknowledging the heavy burdens they shoulder daily as caregivers. It means devising solutions that not only alleviate these burdens but also address the gaps in access, cost, and support. It’s about thinking outside the box to foster collaborations that resonate with the multifaceted lives and interests of women.
By recognizing the influential power of women and tapping into their unparalleled empathy, love, and network, healthcare innovation can truly harness the female engine of product-led growth to make a significant impact.
III. Supporting women & women founders: Are you “Ready for it?”
Investing and innovating in healthcare is investing in women. Vice versa, investing in women requires an investment in healthcare!
So, what implications does this hold for capital allocators and startup support systems?
A statistic often cited is that a mere 2% of venture funding is allocated to women-led startups. This figure is as shocking as it is infuriating, frequently cited as evidence of a male-dominated world or the implicit biases that skew pitch meetings in men’s favor.
But why is this the case? And more importantly, how can we address it?
Several factors contribute to this disparity, such as:
- A low number of female investors in decision-making roles
- Limited access to capital for women
- The prevalence of implicit biases during pitches, where women are often scrutinized more for potential risks than for potential gains.
Efforts to bridge this gap have led to a movement across the ecosystem to increase female founders’ access to capital—from boosting LP funding toward minority and women GP managers to launching VC funds exclusively for women founders, as well as accelerators and incubators designed to equip women founders with the necessary skills and knowledge.
While these initiatives are crucial steps toward leveling the playing field, they don’t fully address the root causes of why men outnumber women as startup founders and why women are less likely to embark on entrepreneurship, despite women outnumbering men in higher education.
The issue isn’t a lack of skill, knowledge, creativity, or risk tolerance among women as women-led startups yield a 35% higher return for investors, with over 60% of such companies being profitable.. The real barrier is our healthcare system, which exacerbates socio-economic gender gaps, affecting women’s health, care quality, and the caregiving burden, ultimately impacting their time, financial stability, and career prospects. A woman’s decision to launch a startup and maximize her full potential must be weighed against the stability of not only her healthcare but also that of her entire family.
“I’m so sick of running as fast as I can, wondering if I’d get there quicker if I was a man” (Taylor Swift)
Supporting more women founders means alleviating the health hurdles and the caregiving burden they face. For early-stage VCs, accelerators, and incubators, support for women founders shouldn’t stop at perfecting pitch decks or facilitating capital introductions. It might also mean providing access to high-quality, affordable healthcare, connecting women founders with financial assistance to ease caregiving burdens, offering affordable childcare, and ensuring better mental health support. Truly supporting women founders involves a comprehensive approach that addresses the unique healthcare challenges they face as “A woman’s health is her capital” (Harriet Beecher Stowe)
In closing, it is personal!
As a healthcare VC and as a woman, it is almost a given that I am passionate and outspoken about the topic of women’s health. For me, it is much more personal than that. Growing up in Vietnam as the eldest of three daughters, I saw firsthand my mother’s dreams and aspirations were put on hold indefinitely after my birth due to the health complications of childbirth and the burden as a mother
For me, women’s health is not just another market map, not just another social issue, not just another thing broken in healthcare we must solve.
For me, women’s health is healthcare for my grandmother, my mother, my aunts, my sisters, my nieces, my future daughter and myself.
Women’s health starts with caring for women beyond their reproductive health, beyond lifting the burdens they face across all facets of healthcare, to start empowering women to pursue their full potential. The foundation of closing the gender inequality starts with investing & improving healthcare for women.
Women’s health is her capital.
Women’s health is healthcare.
Women’s health is equality.
About the Author:

Thea is a Senior Associate at OCV focused on healthcare & biotech. Prior to joining OCV, Thea is a neuroscientist with a PhD from UCLA and an award-winning entrepreneur as Co-Founder of a digital health company enabling precision dermatology leveraging big biological datasets & machine learning.
Thea is passionate about backing extraordinary teams with innovative solutions that are grounded in data & science to make the biggest impact in healthcare.
She is also a passionate Swiftie (and a budding NFL & Kansas City Chiefs fan)!
