Introduction: There’s Something About AI
This past summer, in the backdrop of the historic Tartine Bakery Santa Monica, OCV hosted and moderated a panel discussion (“Generative AI & Computer Vision in Healthcare”) featuring trailblazing entrepreneurs at the forefront of developing innovative AI technologies in healthcare. Sitting in the backdrop of Hollywood and film as an LA-based fund we delve into a movie-inspired primer of healthcare AI insights from our panel and highlight the amazing potential AI can offer in healthcare while being mindful of the challenges and obstacles to its successful adoption and use.
Key Takeaways:
The Myth:
- AI is the new shiny tool that will solve everything in healthcare with more data
The Reality:
- Current healthcare lacks infrastructure and current datasets lack structure, diversity, and have critical gaps for use to power AI
The Goal:
- Use AI to improve healthcare scalability and equity by reprioritizing clinician/scientist time to top of skills and augmenting their abilities
To offer a preview we believe there’s often a misconception that AI and a mass of more data will solve everything when in practice this data tends to be suboptimal and limits the potential, adoption, and outcomes that can be achieved with AI. At OCV we believe in better data enabled by improved infrastructure that allows better control and use of data to develop useful AI products. This will in turn promote better engagement from stakeholders allowing the collection of not only more data, but the right types of data. It is at this point that the flywheel works and each pillar of infrastructure, engagement, and data generation work in harmony to vastly improve healthcare.
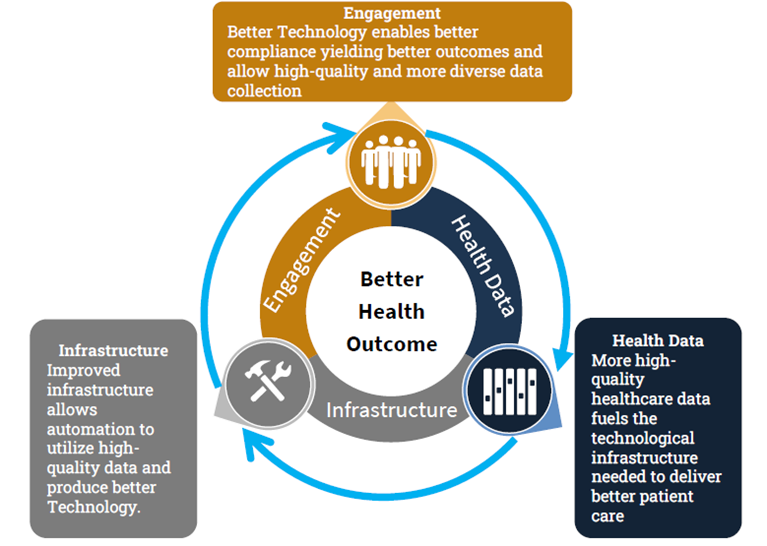
We are strong believers in embracing technology in healthcare and utilizing our diverse skillsets across these spaces to support founders building iterative platforms at this intersection. If you are a founder powering this flywheel we’d love to speak with you!
Apocalypse Now: The Dire Need for Technological Advancements in Healthcare
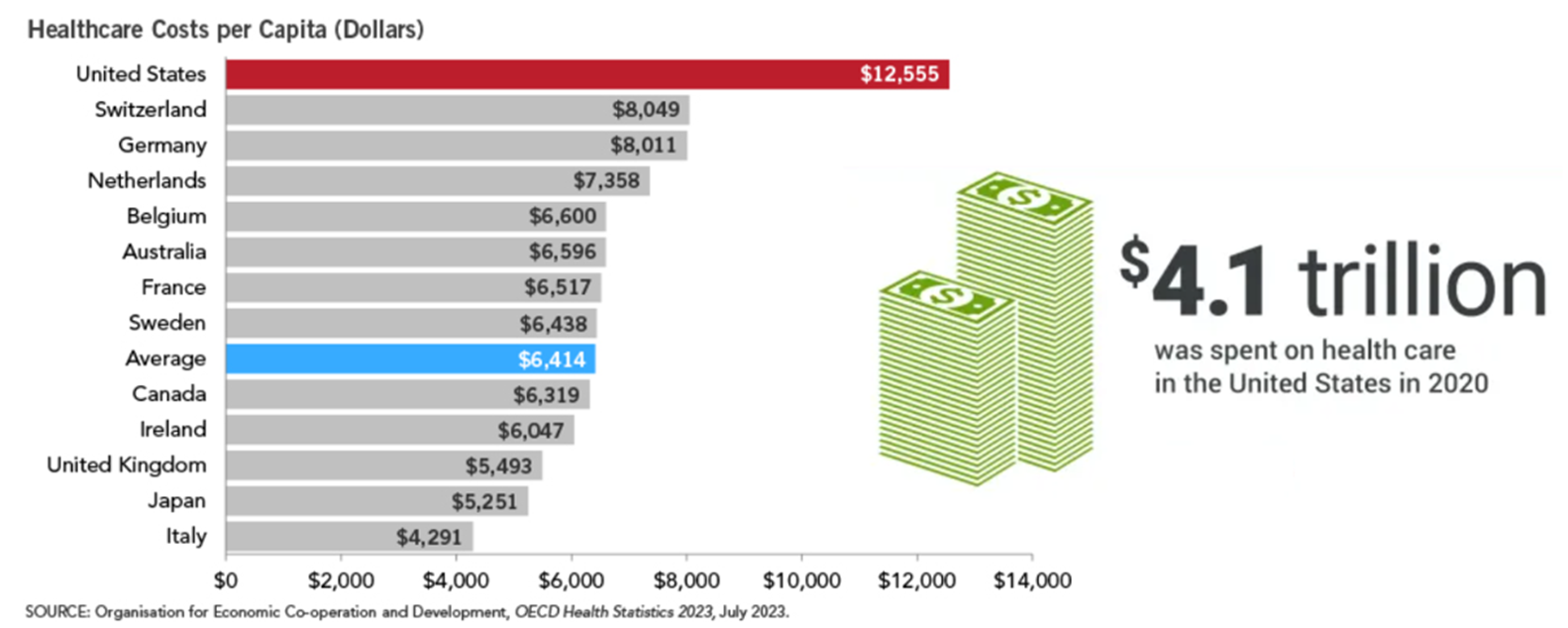
For those who’ve been around the industry, you’ll be very aware of the upcoming sobering statistics, but for those unfamiliar, it’s not great… The US has provided a definitive case study that more healthcare spending doesn’t translate to better outcomes with our nation falling far behind in life expectancy to our peers despite almost double the average Health consumption expenditures per capita ($12K US vs. $6.1K OECD country average). With healthcare spending projected to increase from the current $4 trillion to $7 trillion by 2031, and increasing projected shortages of healthcare professionals, there is an urgent need to enhance care delivery and optimize resource utilization. Without a doubt, the most alarming issue is with the poor status quo that our overtaxed health system yields the worst results for our most vulnerable and underrepresented populations. People of color and other underserved groups face so many disparities in healthcare I’d run out of space trying to list them here. Whether it be life expectancy, disease survival, or just general health outcomes, if you aren’t a white male you are likely to be on the wrong side of the statistics. More so these health inequities are avoidable massive economic burdens costing upwards of $451+ billion in 2018 and warrant investments to promote health equity for disadvantaged racial, ethnic, and education populations. There is no overnight fix for our US health system, but we at OCV see the intersection of healthcare and technology as a major step in the journey to take our health system from a slow and reactive “one-size-fits-all” paradigm to a more targeted and personalized proactive approach with technology as the key engine for enabling health equity and improving the status quo.
A Brief History of AI in Healthcare: A Star is Born
By this point I’m sure everyone is aware of the current zeitgeist around AI across all industries, and healthcare is no exception. However, AI is by no means new to the healthcare space and crude versions have been in use as early as the 1960s in automating scientific analysis and clinical decision support. Along the way there have been frequent uses of AI in healthcare across drug discovery, diagnostics, and image analysis just to name a few. Given AI’s long history you may ask yourself what’s the big deal now? To answer this you just have to look at recent advances in the last 10 years; 2014 – GANs (generative adversarial network), the introduction of transformers in Google’s seminal paper in 2017, and advancements in self-supervised learning that have ushered in the era of Foundation Models which include Large Language Models (LLM’s) like ChatGPT. Foundation Models first defined by Stanford HAI are AI systems trained on massive amounts of internet data including text, images, videos, and more allowing them to be adapted across a wide variety of tasks instead of one model for just one task. With large quantities of data, Foundation models can utilize advancements in self-supervised learning to utilize easier-to-access unlabeled data rather than meticulously curated datasets and then utilize “transfer learning” to adapt to specific new tasks. Thus is born the ability to create one model that can yield many different models with strong potential in healthcare described in a great read by Stanford HAI here driven by advancements including:
Transformer Architecture:
- A super-smart language machine looking at entire sentences, not just individual words, and understands language more like a human does.
- Expedites the creation of LLMs by performing many language-related tasks in parallel (Parallel Processing) allowing for faster training.
Transfer Learning and Pre-Trained Models:
- A key technique, where models pre-trained on massive datasets for specific tasks are fine-tuned for more specialized tasks.
- Highly effective in computer vision, natural language processing, and other domains. Models like OpenAI’s GPT-3 and Google’s BERT exemplify the success of pre-trained models.
Self-Supervised Learning:
- Leverages easier to obtain unlabeled data for training. Models are trained to predict certain parts of the input data, forcing them to learn useful representations.
- Shows promise in various applications, including image and language understanding and is crucial to multimodal approaches (text and images together).
It is these advancements that not only make ChatGPT possible but also dramatically improve what we are able to do with AI models which are well suited to address the data challenges we call out below. If implemented correctly, AI offers significant potential for automating, augmenting, and accelerating care delivery, quality, and equity. It’s important to call out that though Foundation models like LLMs have gotten scary good with Frankenstein-esque calls of “its alive”, they are in fact not sentient thinkers but ultra-complex pattern matchers. Look no further for proof than the issue of hallucinations in LLMs meaning instances when LLMs “imagines” or “fabricates” information. While this might be an annoyance in personal ChatGPT factoid checks, it is potentially life-threatening in the healthcare setting and demonstrates the need for comprehensive regulatory oversight of how AI is developed and used in healthcare.
Potential of AI In Healthcare: Everything, Everywhere, All At Once
On our panel we discussed ways AI can have an immediate impact with its ability to not only add automation to manual processes but also allow comprehensive data utilization yielding opportunities:
Time Reprioritization – The low-hanging fruit of AI is reprioritizing time so highly educated, trained, and specialized healthcare professionals can spend more of their time on crucial tasks.
- Automating laborious manual tasks. Health teams treating patients instead of admin work, scientist designing experiments and theses instead of manually managing papers and reports. In a time where many Physicians are spending more time on admin work than patient care, AI can be a game changer. Look for no further proof of excitement here than the massive venture dollars that have gone into AI medical scribing and medical coding/billing companies.
- Proactive solutions to problems including triaging high needs to help alleviate the overburdened workforce.
A great example of both these concepts is offered by our panelist Ophir Tanz’s company Pearl building the future of dentistry powered by AI. They use AI to enable ROI generating clinical performance insights automating the manual tracking process, as well as offering cutting-edge computer vision like their FDA-approved Second Opinion that increases dentists’ diagnostic accuracy by as much as 37 percent, eases the diagnostic burden on dentists, and helps dentists to identify the early signs of some pathologies that are otherwise difficult to visually detect allowing proactive treatment.
Scalability Enhancement – AI’s grand slam is its ability to see everything, everywhere, all at once. Providing Physicians and Scientists alike the tools to keep up with rapidly evolving literature with real-time meta-analysis and have every available datapoint including troves of personalized patient data considered in decision-making.
- AI’s ability to analyze comprehensive data at unparalleled speeds means more personalized approaches in patient care and more targeted approaches in research.
- Implementation of neural networks and deep learning means unique findings from connections of billions of parameters can help advance care and research in novel ways.
- AI lends itself well to be equally deployable in the top tier metropolitan hospital as well as the rural small private practice if done well allowing parity in the quality of care.
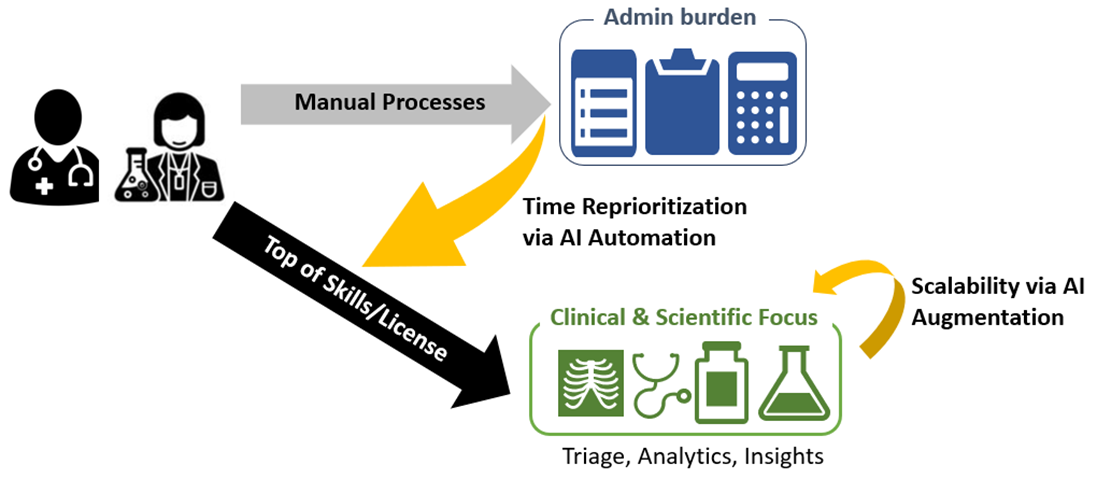
A leading point of our discussion with the expert panelist was dispelling the myth that AI is here to remove humans from the equation. Many of these startups are helmed by Physicians, Scientist, and healthcare operators who grew tired of the clunkiness in healthcare preventing them from helping more patients and providing better care. In short, we’re not building toward robot doctors! Look for no further proof than the sentiment of our panelist Dr. Vivian Chu, Co-Founder of Diligent Robotics, who are building an AI enabled robot whose goal is not replacing but assisting hospital staff with non-patient facing tasks so care teams can focus on what they do best: patient care.
Another great example from our portfolio and one of our AI panelist, Rad AI Co-Founder Dr. Jeff Chang who holds the distinction of being the youngest radiologist on US record and practiced for over a decade prior to starting his vision to dramatically improve radiology workflow with AI. Go to their website and you will quickly see they are leveraging a best-in-class proprietary LLM to allow generative AI in radiology that partners with the Radiologist (not replaces!) and helps automate workflow efficiency, enhancing the quality of patient care, and reducing physician burnout (the giant elephant in healthcare!). 44% of physician experience symptoms of burnout according to survey published in JAMA. AI has the potential to alleviate burnout by reducing the administrative burden on clinicians, allowing them to spend more time working with and for patients.
Furthermore, mounting evidence continues to emerge showing how AI can unburden our overtaxed system. In a recent publication from The Lancet, a real-world instance of AI streamlining diagnostic processes in a 55,000 patient prospective study demonstrating Insight MMG, an AI powered algorithm produced by Lunit, allowed slightly improved cancer detection with a single radiologist + AI compared to the gold standard of two independent radiologist reading mammography scans. Simply stated the results showed 4% increase in cancer detection while also allowing a 50% reduction in reading time directly addressing physician shortage issues. Another interesting finding is there’s a synergy from having both a human physician and an AI to increase sensitivity of abnormal detection. This study lends credence to the statement that AI will not replace doctors but doctors using AI will replace those who do not.
The Data Challenge in Healhtcare: The Good, The Bad, and The Ugly
If AI is the vehicle that propels healthcare forward, then data certainly has an argument as the fuel to make the engine work. It has frequently been said “Data is the new oil” and much like tycoons of old there has been a clamoring to amass vast quantities of it with the promise ‘more is better’. The healthcare industry is a willing supplier generating a massive amount of data, contributing to approximately 30% of the global data volume. Research by RBC Capital Markets predicts that the healthcare industry’s data volume will continue to expand at a compounded annual growth rate of 36% through 2025. This explosion is driven by increased data creation in a myriad of diverse sources such as electronic health records thanks to the HITECH act of 2009 and 21st Century Cures Act, growing data repositories like medical imaging and lab analyses, and new data sources like wearable devices. In addition, the realm of medical knowledge is reported to double every couple of months, and over 5,000 peer-reviewed scientific papers are published daily. So, with this abundant fuel source you may say we’re all set and ready to launch right?
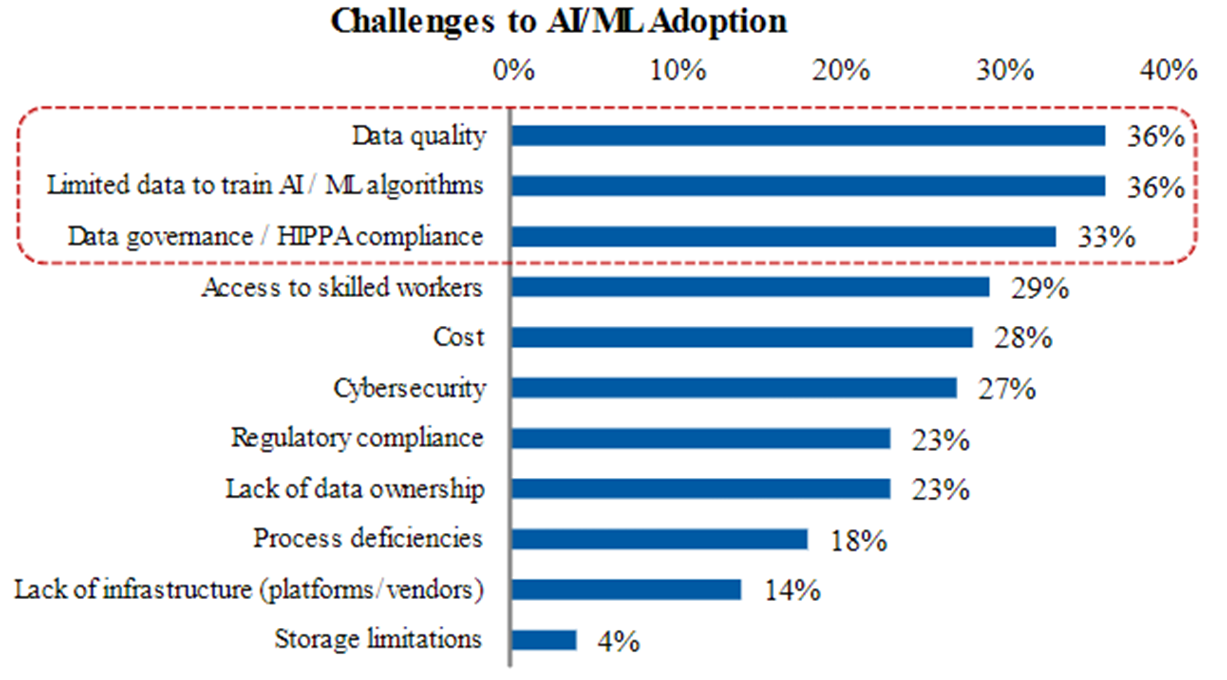
Not quite. Despite this massive amount of data it remains one of the biggest challenges and barriers to adoption. In a Morgan Stanley AlphaWise survey of ~100 senior healthcare executives, data made up the top three responses for challenges and barriers to adoption of ML/AI. Some 1st principles always remain true and the adage “garbage in garbage out” has never been more powerful than in the case of models trained on big data. Concepts on preparing and utilizing data in training AI is a topic deserving a whole textbook or three by itself, but to set the stage there are some high-level issues that serve as limiters to the aforementioned data sources:
|
Source: AlphaWise, Morgan Stanely Research |
INACCESSIBLE DATA: Data not found. To continue the “data is oil” analogy, our healthcare data at the current state is “crude oil” that needs significant refinement and processing before it can be useful to fuel any engine. In an industry where fax is still growing it is no surprise that precious healthcare data are stored in fading manila folders collecting dust in some forgotten hospital shelves or doctors’ offices. Even in the case of digital health data, there exist a large issue of siloed data due to lack of infrastructure that if you’ve ever seen more than one Doctor you are likely acutely aware of having to play connector as the patient.
SUB-OPTIMAL FORMATS: A second stop-gap is having data in sub-optimal formats. You’ll often hear the term of “structuring the data” which simply put is making sure its digestible by any training algorithm being employed. The difference between structured data and unstructured data is like the difference between Excel sheet (accurately labeled and stored) vs a scrapbook (collective stream of thoughts). Needless to say, majority of our healthcare data is still in “scrapbook” era: cute for a while but chaotic, unsearchable, and unscalable. Think about it, would you prefer to evaluate your spending in a scrapbook or an excel sheet with categorized columns and rows?
LACK OF DIVERSITY: Diversity is multifaceted here and is a problem for race, gender, and data geography. Data needs to reflect how and who the product is used on to be useful and at a time when AI can offer some shortcuts it’s important to be vigilant. Our panelist Dr. Matt Michelson, CEO and Co-Founder of ReadoutAI, offered great comments on matching data to real world use and you can view him speaking about it here. The current healthcare dataset is siloed and lop-sided towards the Caucasian male population and won’t be helpful to improve healthcare for the general population, especially underserved communities whether it be racial or socioeconomic. To continue with our “oil” analogy, even after all the filtering and structuring, we have a “useable” oil product that might be appropriate to only fuel cars but not rockets. The lack of diverse representation (See FDA 2020 Drug Trials Snapshot Report) in clinical trials an issue announced by the FDA itself is a powerful example of how our understanding of how different populations may respond to treatments is limited due to initial biases. Overly homogenous healthcare datasets shockingly lead to poor treatment paradigms for as you would guess, everyone else. A clear example of this is despite women making up half the population, women are twice as likely to experience adverse events from drugs, have double the rate of failure in medical implants, and are 50% more likely to be misdiagnosed for heart attacks. Suffice to say you can collect unlimited healthcare data, but if it’s not representative of the patients you are trying to treat it will not improve outcomes.
UNTAPPED DATA: As a final point, there also exists new and emerging data to be collected that previously we lacked the capabilities to collect. There has been an enhanced ability to collect longitudinal data with the proliferation of new modalities like wearable sensors, at home testing, remote patient monitoring, and telehealth. This yields an unparalleled opportunity if leveraged to shift to more proactive care as we interrogate large data and dynamic data signals rather than static disparate timepoints. A great example of this is the advent of continuous glucose monitors in treatment of diabetes with real time data accessible through the cloud compared to the prior standard of test trips done manually only a few times a day. With this type of access we can better test treatments for diabetes and pioneer completely new treatment options that would otherwise not be possible. In this particular case, the idea of real-time insulin adjustments becomes feasible with technology. Like this example in diabetes, there are likely countless others that the collection of new insights will pioneer completely new treatment paradigms not previously accessible. At OCV we believe in better data and that has made us bullish on investments like OCV portfolio company Ozette working to unlock the secrets of immunology leveraging AI that allows bucking the standard low resolution manual workflow in favor of unbiased computationally driven analysis revealing novel insights spurring drug development.
Addressing Concerns of Bias: No Country for Bad AI
For AI to innovate in healthcare, it will replace highly regulated technologies and thus will need to be able to fit within current existing compliance standards. A crucial question we asked our expert panelist is how do we avoid bias in AI and who should be the regulators of training datasets in AI? Point blank the black-box nature of AI is what makes it truly powerful, able to reveal insights and connections otherwise unperceivable. However, without the ability to specifically interrogate all the decisions a black box approach makes to get to its results, an added emphasis is needed on the data inputs to control for potential sources of bias. Remember here that AI models are unique as well in that change over time is a feature not a bug, but that adds more complexity in preventing undesired outcomes.
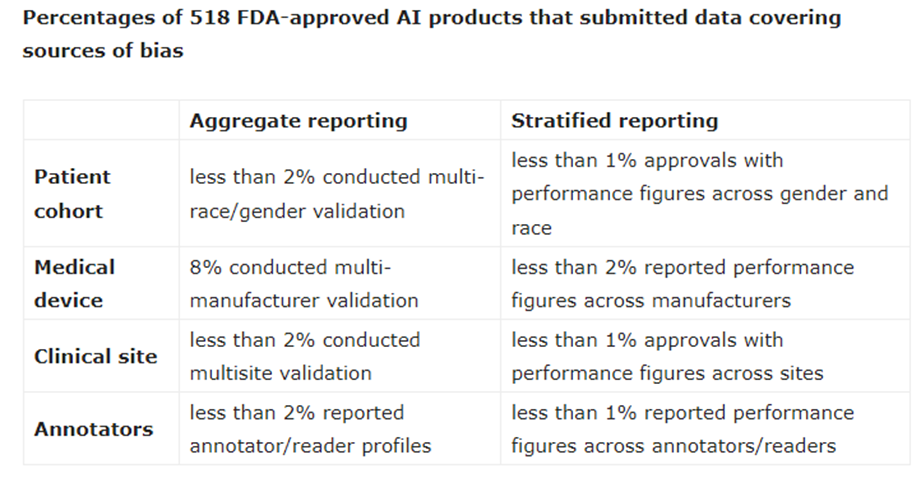
The FDA has already approved over 500 AI based medical technologies under its 510 (k) program that clears a product is substantially equivalent or better than an already used existing approved approach. However, an excellent review of submissions for these 500+ products revealed alarmingly that there was high prevalence of sources of bias across patient cohorts, manufacturer validation, clinical site controls, and annotators. This harkens to our initial point that more data isn’t the end all be all, but more of the correct types of data. The authors make a strong point we highly support that the data going into the training and validation sets is every bit as crucial as the output results and claims.
|
Source: Work by Enes Hosgor and Oguz Akin found here |
Any lack of adequate controls here will lead to continued poor outcomes and potentially at broader scale as removing bias from AI once introduced becomes an immense challenge. Look no further into possible risk here than historical medical precedents like the massive damage Thalomide issuance had on pregnant women due to missing proper controls. In tech we’ve already seen many examples of bias run amok in AI from Amazon’s sexist hiring AI, Computer vision that’s non-functional on people of color from HP and Microsoft, and speech recognition AI like Siri and Alexa biased against multiple underserved groups. It’s not hard to envision in the case of healthcare a biased AI suggesting unnecessary and damaging treatments or withholding lifesaving recommendations in populations not represented adequately in datasets used in its training because examples are already popping up.
Regulators, such as the Food and Drug Administration (FDA), will need to play a vital role in overseeing the training datasets and ensuring the safety and efficacy of AI in healthcare. We are encouraged by the FDA signifying the importance of improving AI regulation with their draft guidance released earlier this year and added emphasis on data (training, tuning, and testing) as well as companies plans to monitor their algorithms over time (predetermined change control plan) to ensure continued positive outcomes. Compared to static technologies of the past the latter is a key differentiation in these new AI approaches which continue to evolve after deployment as they collect more data altering their performance. Collaborative efforts between the industry, regulators, and healthcare professionals are essential to address bias, establish ethical guidelines, and ensure that AI technologies are deployed responsibly and live up to the Hippocratic oath “First, do no harm”.
Conclusion: Dr. Strangelove Or: How I Learned to Stop Worrying and Love AI
At OCV, we firmly believe in the transformative potential of AI in healthcare and a tremendous opportunity for value creation with leading companies able to acquire significant vertical-specific data moats. Addressing the challenges of data access, bias, and regulation is crucial to realizing the full potential of AI in healthcare with a promise of enhanced engagement, improved care delivery, and ultimately putting the “care” back in healthcare. We are at a crucial time now to setup the foundation so AI is an equalizer that improves not only the status quo of healthcare but also the equity in a way only it can.
Adoption of AI in healthcare is still an obstacle to overcome, and on our panel we discussed the challenges faced. In order to change AI adoption the following pitfalls need to be avoided by aspiring entrepreneurs:
- Data Tsunami – creating more work for Physicians rather than providing actionable streamlined solutions
- Non-integrated point solutions – creating larger integration burden than value-add
- Technology Misalignment – cool tech without a clear and measurable ROI use case in a must solve pain point
- Trust – Overpromising and under-delivering with false claims creates a technology stigma. See “Imaging AI vendors’ marketing hype doesn’t always match materials submitted to the FDA”
In this rapidly evolving era it’s easy to get blinded by just how cool AI is and forget about the clinicians and patients we are trying to help. To put an anecdote to this: one of our team members returned from the Vive healthcare conference, whose conference halls were packed with clinical decision support AI companies (that collectively raised over $2B in venture funding in the last few years) to excitedly tell her physician husband about all the cool technology she saw. Her husband, a practicing physician at Cedars Sinai, top-tier medical center and the second largest metropolitan area in the US stared blankly at her and asked “What exactly is clinical decision support?”.
Healthcare doesn’t need flash and AI marketing hype, but instead wants ROI-driven product focused AI addressing real problems. We may have obstacles to overcome as we are in the early innings of an AI paradigm shift, but as often is the case, we tend to over-estimate what technology can do in the short-term but under-estimate what it can do in the long-term. With the promise AI has already shown there’s no better time to be building or investing in the space.
About the Authors:
Chris is a Partner at OCV focused on healthcare investments. He holds a Ph.D. in Pharmacology and has over a decade of interdisciplinary research experience including publications in top journals across Drug Metabolism, Physics, Neuroscience, and Chemistry. He was recognized by Biocom in 2021 as one of ten life science trailblazers under the age of 40.
Thea is a Senior Associate at OCV focused on healthcare & biotech. Prior to joining OCV, Thea is a neuroscientist with a PhD from UCLA and an award-winning entrepreneur as Co-Founder of a digital health company enabling precision dermatology leveraging big biological datasets & machine learning.